THE PAP SMEAR
The number of lives saved by the routine use of the “Pap smear” over the last sixty to seventy years probably runs into the millions. The simple and relatively low-tech procedure has had an enormous impact on public health. Behind it is an interesting story.
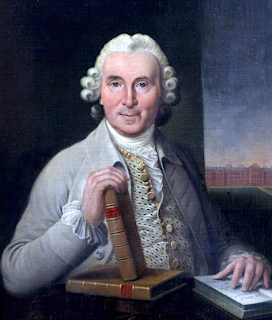
George Nikolas Papanicolaou was born in 1883 in the charming Greek town of Kymi on the island of Euboea. His father was a physician and mayor of the town. After a liberal arts education, George attended medical school, served in the military, earned a PhD in biology in Germany, and decided on a life of
 |
| Papanicolaou as young man (Wikipedia) |
research rather than the practice of medicine. On return to Greece from Germany, George met and married Andromache Mavroyeni. After a short stint on an oceanographic research vessel, George served medically in the Balkan War of 1912 against the Ottomans, during which he met Greek-American volunteers who encouraged him to go to America to seek a scientific career. He decided to take their advice.
He and “Mache” arrived in New York the next year with no job, no contacts, no knowledge of English, and $250. George worked at Gimbel’s department store selling rugs and, being a good violinist, earned extra cash playing at restaurants. He eventually contacted Thomas Hunt Morgan, the famous geneticist at Columbia University, who helped him obtain a position as a technician in the anatomy department at Cornell Medical College, with Andromache as his assistant. George investigated the role of the X and Y chromosomes in determining sex, a problem still under exploration at the time. Studying guinea pigs, George needed to obtain ovarian eggs at the precise time of ovulation. He examined samples of guinea pig vaginal discharge daily and discovered that the smears could accurately determine the day of ovulation. To see if similar changes occurred in humans, he turned to his wife, who became the first person to have a “Pap smear”, and he enrolled volunteer workers at the New York Women’s Hospital. The results demonstrated a similar human sexual cycle.
By chance, a smear from one of the volunteers revealed malignant cells. This generated a study of women with known cancers of the cervix and uterus, showing that the technique might prove valuable in detecting early stages. The findings were first presented at, of all places, the Third Race Betterment Conference in Battle Creek, Michigan, in 1928, a meeting of the eugenics
 |
| Cancer cells shown at Race Betterment Conference (from report of 1928) |
organization founded by John Harvey Kellogg, the inventor of breakfast cereals who worried about “race degeneracy.” The findings generated little interest, however. Papanicolaou, prodded by Cornell’s chief of anatomy and in conjunction with Cornell’s chief of gynecology, embarked on a study in 1939 to do a smear on all women admitted to the gynecological service of Cornell’s New York Hospital. The results made it clear that early cancers, with no symptoms, could be detected accurately, and established a milestone in cancer prevention. The following years were devoted to teaching the methods and refining the techniques for use on a mass scale. The “Pap smear” and an entirely new specialty, cytotechnology, were born.
Papanicolaou was suddenly a famous man. He visited medical centers in Europe, was hosted by the royal family in Greece, received numerous awards and honorary degrees, and gazed at his portrait on postage stamps and Greek currency bills. National Cytotechnology Day, to recognize the value of the technicians who examine the smears, falls every year on his birthday, May 13.
He was nominated five times for the Nobel Prize, though never received it. It is not clear why, but one possibility relates to near simultaneous reports of cancer cells in cervical scrapings by a Romanian, Dr. Aurel Babeș, published in the Proceedings of the Romanian Society of Gynecology of January and April of 1927 and again in April 1928 in Presse Medicale. Babeș was a highly
 |
| Cancer cells from cervical scraping by Aurel Babeș, Presse Medicale 1928 (Hathi Trust) |
regarded scientist in Romania, had his name on over 200 papers, and had published a major work on pellagra. The two sampling methods differed somewhat. Babeș used a platinum loop to scrape the cervix while Papanicolaou used a narrow pipette to obtain free cells and employed a more refined stain. Babeș did not pursue the study of vaginal smears but the presence of the Babeș reports may have caused hesitation by the Nobel committee. Additionally, Papanicolaou’s main supporter at the fifth nomination died just before the final voting. Babeș never contested Papanicolaou’s world recognition.
Incidentally, the uncle of Aurel Babeș, Victor Babeș, had discovered the parasite causing a disease named after him: babesiosis, and was a well-known bacteriologist.
George’s wife, Andromache, was instrumental in his success. She was the “special patient,” who underwent hundreds of vaginal
-%203248%E2%80%933251.png) |
| Andromache and George Papanicolaou (from Exper Therap Med 18, 2019, Creative Commons License) |
smears and was certainly the “most over-tested woman of all time” (Vilos). In addition, she was the breadwinner during the lean years after arrival in New York. She became an expert cytotechnologist and taught the skill to many others, while still finding time to prepare and serve Greek specialties to distinguished guests in their home.
In 1961 Dr. Papanicolaou accepted the directorship of a new Cancer Research Institute of Miami and early the next year the couple moved to Florida. Tragically, three months before the dedication ceremony of May 1962, George Papanicolaou was stricken with chest pain and succumbed rapidly to a failing heart. He was buried in Clinton, New Jersey, next to his niece.
Though he missed the Nobel Prize, the gratitude of millions of women must have been a sufficient reward for the creator of the “Pap smear”.
SOURCES:
Vilos, G A, “The History of the Papanicolaou Smear and the Odyssey of George and Andromache Papanicolaou,” Obstet and Gynecol, 1998; 91(3): 479-83.
Elgert, P A and Gill, G W, “George N Papanicolaou, MD, PhD: Cytopathology.” Lab Medicine2009; 40(4): 245-6.
Papanicolaou, G, “New Cancer Diagnosis.” Proc Third Race Betterment Conference, Battle Creek, Mich., Jan. 2-6, 1928, pp 528-34.
Papanicolaou, G, traut, HF, “The Diagnostic Value of Vaginal Smears in Carcinoma of the Uterus.” Amer J Obstet Gynecol 1941; 42: 193-206.
Albert, P, “George Papanicolaou: Biography,” accessible at: https://library.weill.cornell.edu/george-papanicolaou-biography
Mammas, I N, et al, “Mache Papanicolaou (1890‐1982), the dedicated companion of the great benefactor: An interview with Dr Julie Kokkori, one of the only living relatives of Dr George N. Papanicolaou.” Exp Therap Med 2019; 18: 3248-51.
Tasca, L, et al, “History of Gynecological Pathology XII. Aurel Babeș.” Int J Gynecolog Pathol2002; 21: 198-202.
Naylor, B, et al, “In Romania It’s the Méthode Babeș-Papanicolaou.” Acta Cytologica 2002; 46(1): 1-12.
Diamantis, A, et al, “What’s in a Name? Evidence that Papanicolaou, not Babeș, Deserves Credit for the Pap Test.” Diagnostic Cytopathol 2009; 38(7): 473-6.















%20by%20Gyula%20Kosice%201991.png)