THE EYES HAVE IT: THE EARLY DAYS
OF OPHTHALMOLOGY
For many years, mankind endured diseases of the eyes with little remedy. Infections, especially from gonorrhea and syphilis, cataracts, injuries, and the ravages of untreated glaucoma were prevalent. Physicians had few remedies. Their inexperience was evident when a wave of “Egyptian ophthalmia” swept through Europe and England in the opening days of the 19th century, introduced by Napoleon’s troops from a campaign in Egypt. The disease, now known as trachoma, and characterized by swollen, purulent eyes, eyelashes that scraped the cornea, corneal scarring, and blindness, resisted effective treatment. No department of ophthalmology existed at the time in Europe.
The first university chair of ophthalmology in the world was held by Georg Josef Beer, in Vienna. Beer had studied under the
 |
| Joseph Beer (Wikipedia) |
Maltese anatomist and surgeon, Joseph Barth, who lectured on diseases of the eye. After graduating in 1786, Beer opened a private practice in his small apartment in Vienna focused on eye disease, treating the poor, mainly at his own expense. Twenty-six years later (1812), with no help from Barth, having earned a reputation on his own, he was appointed professor of ophthalmology at the University of Vienna.
Beer produced a two-volume practical text on eye disease. The text, though modern for its time, still cited contaminated air as the cause of purulence and recommended bleeding and leeches as treatments. But the new specialty was established. One of Beer’s pupils, Johan Nepomuk Fischer, founded a
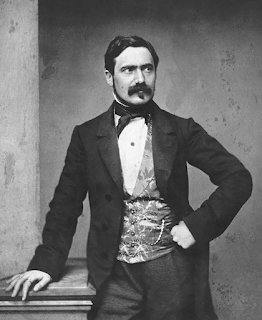
 |
| Ferdinand Arlt (Wikipedia) |
department of ophthalmology in Prague. His assistant, Ferdinand Arlt, the son a blacksmith, had trained in pathology with Carl von Rokitansky, the brilliant pathologist at Vienna’s Allgemeine Krankenhaus. He brought modern pathology and histology to the specialty and after succeeding Fischer in Prague assumed the prestigious ophthalmology chair in Vienna in 1856.
Two discoveries in midcentury dramatically enhanced the profession: the introduction of anesthesia in 1848 and the invention of the ophthalmoscope by Herman Helmholtz in 1851, both huge advances. For the first time doctors could operate without exquisite pain and could peer inside the eye.
The breakthroughs are reflected in Arlt’s three-volume text that grounded ophthalmology on a more scientific basis. First appearing in 1850, the work went through five editions in seven years and included ophthalmoscopic discoveries. Arlt also was the first to elucidate the cause of myopia: elongation of the longitudinal axis of the eye. He improved on methods of removing pterygia and developed new surgical procedures for complications of trachoma.
One of Arlt’s students, Albrecht von Graefe, was awarded the
 |
| Albrecht von Graefe (Wellcome Library) |
first chair of ophthalmology in Berlin. He founded the first journal devoted to ophthalmology, Archiv für Ophthalmologie. Graefe was a kindly man and after his death, three of his colleagues, including Arlt, renamed the journal Albrecht von Graefe’s Archiv für Ophthalmologie in his honor.
 |
| Early Helmholtz ophthalmoscope owned by Albrecht von Graefe (National Museum of Health and Medicine) |
 |
| Von Graefe was well-known in Berlin. This image of him treating a young woman is from a popular illustrated magazine, Die Gartenlaube, 1857 (Internet Archive) |
Franz Cornelius Donders, his friend and professor in Utrecht, invented a tonometer to measure intraocular pressure and elucidated the mechanism of accommodation. His investigations of visual acuity
 |
| Snellen eye chart (Wikipedia) |
and astigmatism led to the proper prescription of corrective lenses. His close associate was Herman Snellen, creator of the Snellen eye charts in use today.
In England, most of the early victims of the trachoma epidemic were military men. In one regiment, 636 out of 700 men were afflicted. John Cunningham Saunders, a young surgeon, on the advice of his superior, Astley Cooper, opened a practice for eye
 |
| John Cunningham Saunders (Wikipedia) |
The European influence extended to America. In 1817 the Baltimore physician George Frick traveled to Vienna to study under Beer and returned to open a practice in eye disease. He published the first American text on ophthalmology, A Treatise on Diseases of the Eye, based largely on Beer’s tome and in use for
 |
| George Frick (From Hubble, A A, The Development of Ophthalmology in America, Internet Archive) |
On their return, the Americans founded two enduring institutions. Reynolds, with a second physician, established the Boston Eye Infirmary for the poor, later known as the Massachusetts Eye and Ear Infirmary, which exists to this day. Delafield and Rogers founded the New York Eye Infirmary, also providing free eye care to the city’s poor. It was the second permanent such institution in America, now affiliated with Mount Sinai Medical School. Both infirmaries were based on Saunders’ institute in London. The AMA recognized the specialty of ophthalmology with the founding of the American Ophthalmic Association in 1864.
 |
| From Hubble, A A, The Development of Ophthalmology in America (Internet Archive) |
Knowledge of bacteriology in the late 19th century allowed prevention and control of eye infections, the next major step toward modern eye care. Advancing technology continues to improve eye care and reduce blindness.
SOURCES:
Lesky, E, The Vienna Medical School of the 19th Century. 1976, Johns Hopkins Univ Press.
Adler, F H, “Sketches from the Life of Albrecht von Graefe.” Ann Med Hist, 1928; 10(3): 284-90.
Rohrbach, J M, “Albrecht von Graefe in the Present, the Past, and the Future.” Graefe’s Archive for Clinical and Experimental Ophthalmology. 2020; 258: 1141-47.
Laios, K, et al, “Carl Ferdidand von Arlt, Ritter von Bergschmitt (1812-1887): A Pioneer in Ophthalmology.” Acta Medica Academica 2019; 48 (3): 331-36.
Ivanisevic´, M, “Prof. Dr. Carl Ferdinand Ritter von Arlt (1812-1887): His Life and Work During his Ophthalmological Career in Prague.” Čes. a slov. Oftal., 79, 2023, No. 1, p. 36–40. (available in English at: https://cs-ophthalmology.cz/en/journal/articles/268
Pearce, J M S, “The Ophthalmoscope: Helmholtz’s Augenspiegel.” European Neurology 2009; 61: 244-49.
Lyle, T K, “Some of the Great Historical Figures Associated with Moorfields.” Brit J Ophthalmology1961; 45: 251-58.
SchmidtiWyklicky, G and Gröger, H, “Georg Joseph Beer (1763–1821). Leben und Werk des Begründers der ältesten Universitäts-Augenklinik.” Spektrum Augenheilkunde 2012; 26: 266-72.
Duke-Elder, S, “Moorfields and British Ophthalmology.” Proc Royal Soc Med 1964; 58 (7): 541-45.
Tower, P, “George Frick: Factors Influencing Early Nineteenth Century Ophthalmology.” AMA Arch Ophthalmology 1958; 60: 989-94.
Kara, G B, “A Historical Review of the department of Ophthalmology at the New York Eye and Ear Infirmary.” N.Y. State J Medicine 1973; 73 (23): 1-10.
Snyder, C, Massachusetts Eye and Ear Infirmary: Studies in its History. 1984; Mass. Eye and Ear Infirmary.