AZTEC CONTRIBUTIONS TO EUROPEAN
PHARMACEUTICALS
When Hernando Cortés and his troops entered the Aztec capital city of Tenochtitlan in 1519 they were stunned. Huge temples and palaces surpassed many of their own. Sweepers kept the streets cleaner than in Spain, and aqueducts carried in fresh water from the nearby mountains. A knowledge of mathematics, astronomy, two separate calendars, and pictorial writing revealed unexpected sophistication. Colorful markets tempted the troops, including one specializing in herbs and medicines, as noted in a letter by Cortés: “There is a street set apart for the sale of herbs, where can be found every sort of root and medical herb which grows in the country. There are houses like apothecary shops, where prepared medicines are sold, as well as liquids, ointments, and plasters.”
Cortés found that the Aztecs enjoyed a well-organized medical system. Physicians, known as ticitl, took care of most ills using a combination of herbals and contact with various gods. Surgeons and midwives also practiced their specialties. Extensive botanical gardens in and near the capital supplied the wide variety of herbals used as medicines. Aztec experts classified and named the plants and doctors prescribed them internally and externally. The Spaniards appreciated the skills of Aztec practitioners sufficiently for Columbus to suggest to Charles V that he need not send additional physicians to Mexico.
A ticitl (robed figure on mat and above) making a diagnosis
(from Codex Magliabechiano, folio 78r, Wikimedia Commons)
A number of these herbal remedies entered the medical practices in Europe. One of the first was tobacco. “Tabaco,” originally the indigenous name for a y-shaped pipe to enable powder of any plant to be sniffed into each nostril (used mainly for hallucinogenics), became the name for the leaf. Columbus had noticed Caribbean natives applying leaves for wounds and illnesses 
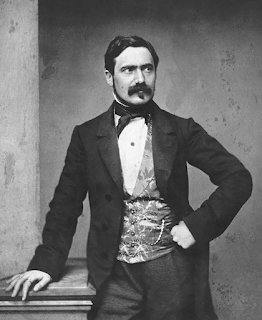
Nicolás Monardes (Wikipedia)
and others observed it being chewed, smoked, or mixed with other plants as poultices. When it arrived at the docks of Seville, the prominent Seville physician, Nicolás Monardes, praised its
marvelous properties in an influential book (first edition in 1565) on medicines from “our West Indies.” The plant grew well in European soil.
In 1560 the French ambassador to Portugal, Jean Nicot, found that it cured a number of ailments, including skin lesions, and popularized it. The French called it Nicotaine (Nicotiana in Latin, now the genus designation), and it appeared in numerous materia medica. Classified as “hot and dry” in 
Jean Nicot (Wikipedia)
terms of Galen, it neutralized cold humors causing various ailments and was used topically and rectally. Nicolas Culpepper praised it in England. Eventually, smoking the leaves largely replaced its use as a medicine.
Monardes also described sarsaparilla, also considered by European medical writers a hot and dry medicine and sudorific. It enjoyed brief popularity as an antisyphilitic but subsequently was used mainly for rheumatism and fevers. It became popular in patent medicines in the nineteenth century (though sassafras was often the main ingredient), was taken for a variety of ailments, and often mixed with alcohol or opium.

Patent medicine ad for sarsaparilla (Wellcome Library)
The cathartic jalap, used liberally by practitioners like Benjamin Rush, was derived from Ipomoea purga, a Mexican plant. Monardes called it “Rhubarb of the Indies” after the cathartic rhubarb, though there is no botanical relation of the two plants. It was used for fevers, coughs, and chronic diseases as well as a cathartic.
The medicine that achieved the most popularity was an extract of the wood of the Guaicum tree (Guaicum officinale), found in many of the Caribbean islands and usually referred to as lignum sanctum (holy wood) or, in Spain, guaiacum. Spaniards had noticed its use by locals for what apparently was syphilis and it soon arrived in Europe for the same purpose. Mercury had been the standard anti-syphilitic,
Ulrich von Hutten (Wikipedia)
used in doses that caused numerous side effects. Ulrich von Hutten, a notable German humanist and supporter of Martin Luther, wrote the first major work on lignum sanctum in 1519. He described his own case of syphilis, how to prepare the wood (a hot water extract), and outlined a treatment that included preparation with a cathartic and a special diet. Perhaps more well-known today is the work of Fracastoro, whose work on syphilis praised lignum sanctum and gave the disease its modern name. The enthusiastic recommendations of Hutten and Fracastoro stimulated a high demand for the wood. But the Fugger family of Augsburg had secured from Charles V a monopoly on guaicum in exchange for a loan. Prices went too high for patients of modest means until 1525, when the monopoly expired. Monardes also considered it helpful against scurvy, rheumatism, and “almost all chronical distempers.” Guaiacum lasted until the early 1800s though mercury persisted for syphilis until the advent of arsenicals.

Right: cutting, measuring, boiling guaiacum.
Left: administrating guaiacum. (Wikipedia)
The Spanish domains yielded other new medicines, some from non-Aztec areas. Extracts of bark of the chinchona tree in Bolivia and Peru were effective against malarial fevers, and eventually yielded the active ingredient quinine. Ipecacuanha root, from Central America, served as an emetic and sweating agent. It was especially popular in an English preparation called “Dover’s Powder,” a combination of ipecacuanha, opium, and potassium salts, used as a sweating agent to ward off colds and other fevers in early stages. Cocaine, from coca leaves chewed by Peruvian natives to allay hunger or for pleasure, came later as an ingredient in tonics, as a local anesthetic, and as an addicting drug. Peruvian balsam served as an aid to wound healing. Bezoars from Peruvian llamas were valued as healing agents, superior to bezoars from elsewhere. Hallucinogens, mainly from mushrooms, did not prove popular as European medicines, though used in Mexico for magical and religious purposes.
By the middle eighteenth century Spain alone was importing about 155 tons of New World medicinal plants annually, supplemented by copious imports from other countries. Many of these products are with us today.
SOURCES:
Gänger, S, “World Trade in Medicinal Plants from Spanish America, 1717-1815.” Medical History2015; 59 (1): 44-62.
Guerra, F, “Aztec Medicine.” Medical History 1966; 10: 315-338.
Estes, J W, “The European Reception of the First Drugs from the New World.” Pharmacy in History1995; 37 (1): 3-23.
Munger, R S, “Guaicum, the Holy Wood from the New World.” J Hist of Medicine 1949; 4: 196-229.
Hope, J, Lectures on the Materia Medica: Containing the Natural History of Drugs, their Virtues, and Doses. v 2. (from manuscript of Dr. Charles Alston)
Monardes, Nicolas, Joyfull newes out of the new-found worlde. Wherein are declared, the rare and singuler vertues of divers herbs, trees, plantes, oyles and stones, with their applications, as well to the use of phisicke, as of chirurgery ..., trans by John Frampton, 1596 (online in Wellcome Library).
A full index of past essays is available at:
https://museumofmedicalhistory.org/j-gordon-frierson%2C-md