FROM SIENA TO NAPOLEON:
A TALE OF TWO ANATOMISTS
The lymphatic system occupies but little time in today’s anatomical studies. Hard to see, the tiny, colorless lymphatic vessels nevertheless are ubiquitous and serve important functions, as described by the anatomist who pioneered investigations into their pathways, Paolo Mascagni. Born in a village near Siena, Tuscany,
 |
| Paolo Mascagni (Wikipedia) |
Paolo studied at the University of Siena. His professor of anatomy, Pietro Tabarrani, noticed his talents, appointed him as prosector, and advised him to study the lymphatic vessels. When Tabarrini died in 1780, Mascagni assumed his chair and explored the lymphatic system intensively. In 1784 the Academy of Sciences in Paris opened a competition for the best work showing lymphatic vessels. Mascagni entered two papers that arrived too late to win the prize. But the Academy, impressed, awarded him a special prize and shortly afterward he published a monumental volume on lymphatics, illustrated with 41 copper engravings. He is credited with discovering about 50% of the lymphatic vessels, showing that they originated from cavities and surfaces, that they all passed through one or more lymph nodes, and that they were separate from the arteriovenous system except at their termination at the thoracic ducts (in contrast to general belief).
Painstaking work was the secret to his success. Using mercury as a contrast agent, he injected it through glass tubes whose finely tapered ends were inserted into lymph vessels. The detailed drawings tell the story (see illustration).
 |
| Thoracic lymphatics, from Mascagni's Vasorum Lymphaticorum (Hathi Trust) |
In 1797, France’s revolutionary army invaded Tuscany, an area under Austrian rule since 1737. Under the French regime, Mascagni reluctantly served as superintendent of arts, sciences, and charitable institutions, fighting against the removal of valuable property to France. When the Austrians regained control, he was branded as a collaborator, jailed, then freed after court battles. In 1801, realizing that his punishment was probably unjust, the University of Florence attracted him by combining the chairs of anatomy, physiology, and chemistry and raising his salary. In Florence he wrote a student’s anatomy text and prepared a series of life-sized wax anatomical models, a popular method for teaching before the introduction of cadaver preservation techniques.
Mascagni passed away suddenly in 1815 of a septicemia. Two years earlier he had taken on a bright student, Francesco
 |
| Francesco Antommarchi (Wikipedia) |
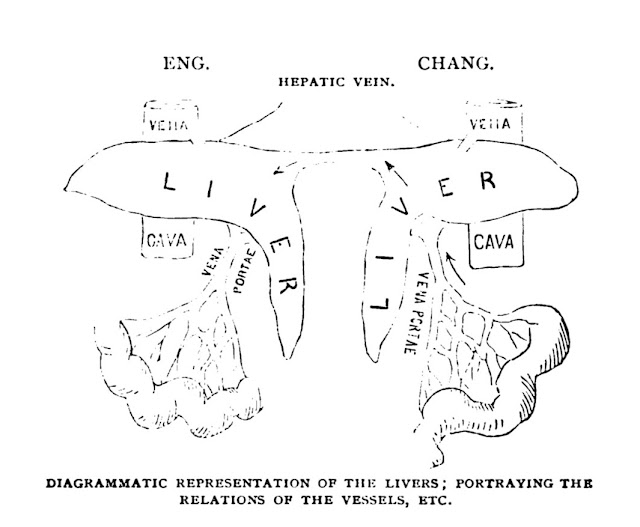
Antommarchi, as prosector. Francesco, born in Corsica, having earned a degree in medicine and a doctorate in surgery, had assisted Mascagni in the preparation of the student’s anatomy atlas. Mascagni’s heirs tasked Antommarchi with putting two unfinished works of the anatomist into publication. One, on histology, was published quickly. The other was Mascagni’s major work, a huge color atlas of anatomy. Before it was completed, however, news arrived that Napoleon, in exile on St. Helena after losing at Waterloo, needed a new physician since the Irish one assigned to him was leaving. Antommarchi, a Corsican like Napoleon and actively promoted for the job by his mother and family, was chosen as Napoleon’s new physician. When he left Florence, Antommarchi took three sets of plates with him, expecting to finish the atlas later.
He arrived in 1815 at St. Helena, an island owned by the British East India Company that was 122 miles from the nearest land. To prevent a second escape by the ex-emperor, six brigs (2-masted square-rigged vessels) sailed around the island day and night, five other armed vessels were kept near the capital, and 2784 military
 |
| Archibald Arnott (Wikipedia) |
men kept watch on land. Napoleon, age 45 and in good health at the time, considered Antommarchi young and inexperienced and intermittently dismissed him, only to reconsider. But to satisfy Napoleon, the British brought a British army surgeon, Archibald Arnott, who had attended the wife of Napoleon’s Grand Marshall, to the island in 1821. By this time Napoleon was ill, losing weight, vomiting intermittently, and complaining of upper abdominal pains. Treatments of calomel, blistering, and the like did not help and Napoleon died on May 5, 1821. An autopsy revealed extensive stomach cancer. Dr. Arnott and Antommarchi both made death masks.
 |
| "Death of Napoleon" by Charles de Steuben. Antommarchi is to left of Napoleon with hand on pillow, seated below him is General Bertrand, an old comrade, whose wife with two children are to the right. A third child peeks behind the pillows. Dr. Arnott is the second head in from the right margin. Napoleon's valet and a servant behind him are framed by the canopy. Click on plate to enlarge. (Painting from Wikipedia. For labels see: https://www.napoleon.org/en/history-of-the-two-empires/articles/who-was-present-at-napoleons-death/ ) |
Meanwhile, the managers of Mascagni’s estate had cancelled Antommarchi’s contract for the large atlas and assigned it to three professors at Pisa. They produced the great Anatomia universa over a period of nine years. The work is a major achievement. Its pages
 |
| Plate from Anatomia Universa Click on pic to enlarge it. (Hathi Trust) |
are roughly 3 x 2 ½ feet in size and many plates are hand colored. The figures are arranged so that, in some cases, three pages, laid together, combine to show a layer (muscles, for example) of a human in life-size. The principle signature on the plates is that of Antonio Serantoni, a known artist and engraver.
Antommarchi, defying a court order, produced his own version of the work, using the plates in his possession. It was not successful, was technically inferior, and lacked a number of figures that appear in the Anatomia. After his publication, Antommarchi was restless. He became an inspector of hospitals in Poland, where he assisted in the 1831 uprising against Russia, but fled to Paris as the revolt failed. From there he moved to Louisiana, then Veracruz, Mexico, and finally settled in Santiago, Cuba, where his cousin owned a plantation. There he acquired a reputation as a skilled ophthalmologist, specializing in cataract surgery. He never married and died of yellow fever at the age of 57, while living in the Governor’s house.
Mascagni’s contribution to the anatomy and function of lymphatics is a lasting one. His Anatomia, however, is now prized primarily by collectors. Modern students turn to their computer screens for 3D anatomy models.
SOURCES:
Eimas, R. “The Great Anatomy of Paolo Mascagni.” Available at:
https://ir.uiowa.edu/bai/vol38/iss1/5/
Di Matteo et al, “Art in Science: Giovanni Paolo Mascagni and the Art of Anatomy.” Clin Orthop Relat Research (2015) 473: 783-8.
Riva, A., et al, “The Evolution of Anatomical Illustration and Wax Modelling in Italy from the 16thto Early 19th Centuries.” J of Anatomy (2010) 216: 209-222.
Wilson, J. B. “Dr. Archibald Arnott: Surgeon to the 20th Foot and Physician to Napoleon.” Brit Med J (1975) August 2, pp 293-5.
Homason, Henry D., Napoleon, The First Emperor of France: Being a Summary of the Facts Concerning the Latter Days of Dr. Francois Antomarchi, the Last Physician to his Imperial Majesty.1910, Franklin Hudson Pub Co., (The spelling of Antommarchi’s name varies)